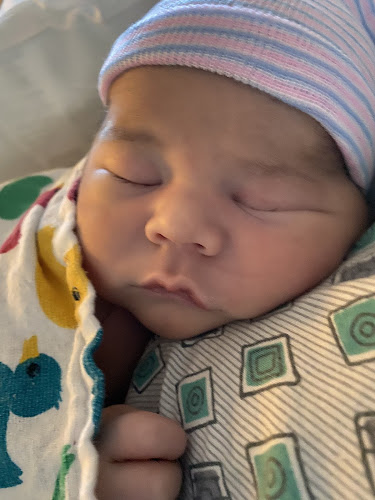
We welcomed our son, Matthew Arrupe, into the world almost four months ago and in this short time, our lives have changed drastically for the better.
All the clichés and warnings about time flying or kids growing up in the blink of an eye are bitter-sweetly true. It’s incredible to see the newness of each day, but hard to say goodbye to those sweet newborn moments and pack away the clothes and diapers he has already outgrown.
I’ve never written a birth story (clearly), and am not even really sure how to go about composing one or what you’re supposed to include (how much is TMI?), but in these few short months I’ve noticed details of Matthew’s birth slipping my mind. So, in an effort to record the memories that aren’t yet lost of that incredible day(s), I’ve decided to write them down – in the middle of the night as I pump for the billionth time.
(Dress | Onesie | Dress Shirt | Pants)
Here we go:
Our sweet little green bean was due on March 25, 2020. Many of our pregnancy milestones had occurred on holidays, so I naturally joked that they would more likely arrive on April Fools.
Well, the joke was on me.
To be fair, based on our fertility charting, we expected that the baby would arrive in early April. I was just hoping my body would get fed up and speed up the process a bit. It did not.
Our due date came and went and based on the (lack of) progress my OB observed in my final few visits, we were scheduled for an induction the day I hit 41 weeks, at 6pm on April 1.
Oh, and did I mention that this all was happening at the beginning of a state-wide shelter-in-place order due to the Covid-19 pandemic? I know they say birth plans should be flexible, and ours was (I thought), but there really was no preparing for this particular bump in the road.
I spent the days leading up to the birth fearful of changes to hospital policy, fearful that my husband, who works in the medical field, would not be able to be with me. I expressed this fear to my doctor at my second-to-last appointment and she assured me that scenario was so unlikely it hadn’t even crossed her mind. By the next appointment, she explained that it was a possibility given what happened in NY, but she and the other OBs were advocating for an exception to be made for Labor & Delivery. I checked the hospital’s new protocols multiple times a day. One conversation with an operator at our hospital left me hysterical as she led me to believe it was very likely I would have to labor alone. Thankfully, that was not the case.
By the time of our induction date, the hospital’s restrictions limited the number of “visitors” for L&D to one person, which meant Michael could be there. On one hand, the policy helped keep our delivery private (which I preferred – sorry mom). On the other hand, our doula couldn’t come either. And since I was being induced, she couldn't help me labor at home and begin the birthing process with the extra support we’d hoped to have.
I didn’t really think I had a birth plan, other than to deliver safely with a few preferences that were pretty flexible in my mind. But when everything is turned upside down by a problem you hadn’t known to create a plan B for, you realize you do, in fact, have a birth plan, and I have to say, a pandemic was not part of mine.
Now, back to the induction:
We arrived promptly at the hospital on April 1, pillow and bag in tow. Upon our arrival, we were greeted by security waiting to check our temperatures and asked us various health questions that I’d answered at several of my last appointments. No sir, I had not left the country at 41 weeks pregnant. I can barely get comfortable in my princess-and-the-pea pillow situation at home and the thought of sitting in an airplane makes my lower back hurt. Thankfully, he also saw the humor in asking me this.
The hospital itself was a ghost town, which was both strange and comforting all at the same time. We were directed to the L&D floor and when we stepped off of the elevator, we were the only ones there. The woman at the desk seemed to not know we were scheduled, which is always reassuring, and had us take a seat in the waiting area for about 20 minutes before we were escorted to a room.
While we were waiting to be brought back, one of the nurses noticed that my chart indicated I planned to deliver without medication and that I had requested the wing of the hospital that accommodated those deliveries (aka the nicer rooms with the bigger beds, birthing pools, and such). This was true. I did want to be there. It sounded great and I intended to labor without medication - mainly because of my intense fear of needles. (During our birthing class we watched multiple vaginal deliveries and I didn’t bat an eye, but just the discussion of the process of an epidural caused my mouth to go dry and the room to spin. I wish I was joking.) I also knew that I have a very low pain tolerance and was open to an epidural if needed and if I could stomach it.
I told her that I was planning to labor in that wing, but because I was being induced and heard Pitocin made things more intense, I didn’t want to cause extra work for them should I need to switch and would stay on the main L&D floor.
I should have gone to the bigger room.
The nurse took us back to a room that I later learned was for triage until they had my actual room ready. It was a small room with a tiny bed and a chair for Michael to sit in. No windows, no TV, and barely enough room on each side of the bed for a person to walk by. It was. . . cozy.
We were there for six hours before they finally moved us to a normal room. In the first three hours, my belly and I were hooked up to the monitor, I had the IV port put in my hand, and we had three different people ask why I was in that room the moment they walked through the door. That was it.
When a doctor finally came to check how far along I was (less than 1 cm), they started me on my first dose of Cytotec buccally (in between my lip and gums). Each round of Cytotec lasts around 3 hours and this first round had no effect on me.
At the 6 hour mark I still hadn’t had one contraction, but they did finally have our room ready.
After settling into the new space at around midnight, the doctor mentioned she would like to try a Foley bulb to begin manually dilating me. I didn’t know much about the procedure other than it was very painful (which the doctor also emphasized), but didn’t want to use that method of intervention unless absolutely necessary, so I declined and she got me going on my second round of Cytotec, this time vaginally, and I finally started to have contractions.
I ended up having three rounds of Cytotec total (1 buccally, 2 vaginally), but even after six hours of steady contractions, I had not progressed at all. The doctor, who had been pushing for a Foley bulb with each check, again suggested the intervention, and I agreed. We needed to do something to get things moving.
Around 7am, a new doctor came in to talk me through the procedure. She was gentler with my feelings and seemed to better understand my fear. After another explanation of what the Foley tube was and how it worked, she began while Michael held my hand and encouraged me through the process.
It was awful.
It was honestly the most painful part of the delivery for me, and (spoiler alert) I pushed a child out of me. I cried the whole time and when it was over, they found that something had gone wrong. The bulb wasn’t where it needed to be and they were going to have to do it all over again.
So, I cried some more.
It was near 10am when she came back, stripped my membranes (not pleasant), and inserted a new Foley. The procedure was still painful, but did not feel as traumatic, which I attribute to having better context of what to expect and a full belly.
I continued to contract and the Foley Bulb fell out at around 2pm which meant I was about 4cm dilated (finally).
At this point, it had been about 20 hours since I’d been admitted and I was having around 3 contractions every 10 minutes. Baby’s heart rate had been wonderful since we arrived and while I was feeling strong, I was also exhausted. My nurse had been checking in with me regarding pain levels, and I told her I was at a steady 6-7. My contractions were honestly not that bad. The pain was similar to menstrual cramps I’d experienced before, but while on my period there was a longer time of relief between the intense cramping.
The nurse had also begun bringing up the option of an epidural, which again, I was not opposed to, but still very fearful of. She ended up having a conversation with M while I was in the restroom and he better articulated my fear of needles, which helped her to better understand where I was coming from. She explained what she was noticing in regards to my exhaustion and that our next step of Pitocin was only going to add to it all.
I knew this. Pitocin and its intense effects had been
on my mind too. I was also very aware of the constant contractions, their
effect on my energy levels, and that I had gotten little to no sleep so far.
I also knew I wasn’t even halfway dilated which meant there was a lot of time
left. So, I decided to hear about the epidural again and after some sweet coaching
with that nurse and M, we called the anesthesiologist and requested the
epidural.
Michael wasn’t allowed to stay in the room with me (even after trying to persuade them otherwise), but I did have another sweet nurse, who’d just begun her shift, there to hold my hand. The anesthesiologist was incredibly nice and walked me through every step of the process. The initial numbing shots stung a bit, and trying to stay still while contracting was challenging, but I made it through.
And it was glorious. As was the sleep I was finally able to get.
The Pitocin started to speed up the process, and around 5pm my nurse checked me and said I was far enough along for the doctor to come and break my water. (I forget how many centimeters I was at that point.) Mike and I were so excited to hear that. After what seemed like the slowest labor ever, we were making moves and getting closer to meeting our baby.
We waited over 5 hours until a doctor finally came by to officially check my progression and break my water and during that time our new nurse (after another shift change) had barely spent time in the room. It was similar to the way we’d been treated at the beginning of the induction, but this time I had been laboring for over 24 hours. It was incredibly frustrating and both Michael and I were visibly upset about the delay and expressed our feelings with the doctor who didn’t seem to think there was a problem with making us wait so long either time since the baby was not in any distress.
I’m still trying to give the hospital the benefit of the doubt and hoping this treatment had to do with limited staffing via Covid-19. I understand that labor requires a lot of waiting around, but we were not informed properly and I don’t think there should have been such a long gap in having a doctor come to my room.
Frustrations aside, the doctor finally broke my water at around 10pm. There was meconium present which meant the baby had pooped in utero and would need some extra care when they arrived. Apparently this is fairly common, especially in babies that come past their due date, but it was still scary to me, and in my exhausted state I couldn’t help but wonder if things would have been different had we not been left unchecked for so long. (This was totally the exhaustion and fear talking and probably not the case, but the thought still crossed my mind.)
Thankfully, at about 11pm the doctor checked me again and let us know it was time to start pushing. For some reason, my body did not respond to this news very well. I all of a sudden had crazy chills and shakes (which is apparently normal and has to do with hormone changes during delivery) and I threw up (which I guess is also normal).
Once I was more calm, the nurse let me know what this next step would look like and got me into pushing position. Michael and I asked if she thought we’d have the baby that night (April 2) or the following morning (April 3) and she was optimistic, but pretty convinced we were not having this baby that night.
Challenge accepted.
The nurse and Michael each had a leg in hand while she calmly counted to ten for each push. My asthma made it harder to actively push during the full count. I consistently hit 7 or 8 and had to stop to catch my breath. But y’all, I was determined to get that child out of the womb and into my arms.
I don’t remember how many times I pushed, but after around
30 minutes (which included a “break” for the rush of hospital personnel to get
there) our baby was born and Michael announced, both proudly and surprised,
that it was a boy.
Born April 2, 2020 at 11:39pm.
8lbs, 11oz, 20 inches long, and a bundle of pure joy.

Peace,
Sarah












No comments :
Post a Comment